5.1 Human well-being critically depends on a healthy environment
Human health and well-being are intimately linked to the state of the environment. Good quality natural environments can provide multiple benefits to physical, mental and social well-being. However, environmental degradation — such as that caused by air and water pollution, noise, radiation, chemicals or biological agents — can have negative effects on health.
Despite substantial improvements in recent decades, environmental health challenges remain considerable. In addition to established problems — such as air pollution, water pollution and noise — new health issues are emerging. These are associated with long-term environmental and socio-economic trends, lifestyle and consumption changes, and the rapid uptake of new chemicals and technologies. Furthermore, the unequal distribution of environmental and socio-economic conditions contribute to pervasive health inequalities (WHO, 2012; EEA/JRC, 2013).
Human-induced environmental phenomena, such as climate change, depletion of natural resources, and biodiversity loss have potentially wide-ranging and long-term effects on human health and well-being. Their complex interplay calls for integrated analysis of the relations between environment, health and our systems of production and consumption (EEA/JRC, 2013; EEA, 2014i).
As an example of systemic analysis, the ecosystem-based perspective links human health and well-being with the preservation of natural capital and related ecosystem services (EEA, 2013f). Although very promising, ecosystem-based approaches are still hampered by knowledge gaps and uncertainties. Information exists on certain specific themes, such as air pollution, noise, water quality, and some hazardous chemicals, but understanding of the interaction of multiple environmental pressures in combination with social and demographic factors is currently limited.
Human health and well-being are intrinsically linked with the quality of the environment. A range of detrimental health effects have been linked to environmental pollution and other forms of environmental degradation, and the health benefits of a high quality natural environment are increasingly recognised. This chapter provides an insight into the impacts on human health of climate change and other environmental factors. It highlights the evolving nature of environmental challenges to health and well-being, and what this means for how we address these challenges.
The sections of this chapter are structured around the following aspects of the relationship between environment, health and well-being:
- reflections on how environmental conditions, demography, lifestyle, and consumption patterns interact to affect health in Europe (Section 5.3);
- impacts of specific environmental issues, such as water pollution, air pollution, and noise on human health (Sections 5.4, 5.5 and 5.6);
- human health and well-being considerations in the context of complex systems, such as urban environment and climate change (Sections 5.7 and 5.8);
- reflections on the need for new approaches to address complex environmental challenges and emerging risks (Section 5.9).
5.2 European policy takes a broader perspective on the environment, human health and well-being
Concerns about human health and well-being are powerful drivers for environmental policy but have primarily been addressed through separate approaches dealing with air quality, water quality, noise and chemicals. Since the finalisation of the EU Environment and Health Action Plan (EC, 2004a) in 2010, there has been no dedicated environment and health policy in the EU.
Implementation of the existing environmental policies is likely to reduce specific health burdens further, but the need for more systemic approaches to reduce health risks is recognised in recent EU policies. The newly amended Environmental Impact Assessment Directive strengthens the provisions for assessing and preventing risks, including to human health (EU, 2014a).
Priority objective 3 of the 7th Environment Action Programme is 'to safeguard citizens from environment-related pressures and risks to health and well-being'. It addresses air quality, water quality, and noise, and announces an EU strategy for a non-toxic environment, to be supported by a knowledge base on chemical exposure and toxicity. Furthermore, it considers the health impacts of mixtures of chemicals, and risk management of new and emerging issues, such as endocrine disrupting substances and nanomaterials (EU, 2013).
Chemicals policy is a particularly important area when it comes to health and the environment. The main 'horizontal' chemical policy, REACH (addressing the registration, evaluation, authorisation and restriction of chemicals) (EU, 2006), includes a range of measures to improve the protection of human health and the environment. However, the regulation does not address the problem of simultaneous exposures to multiple chemicals. Driven by growing evidence and societal concerns, further legislative work is foreseen on this issue (EC, 2012c), as well as on the issue of endocrine disrupters (EC, 2012d).
Promoting good health and reducing inequalities, a central theme in EU health policy (EC, 2007b; EU, 2014b), is also an integral part of Europe's smart and inclusive growth objectives (EC, 2010).
At the international level, the World Health Organization pan-European Environment and Health Process addresses environment and climate-related threats to human health, particularly in children (WHO, 2010a). The new World Health Organization health strategy for Europe considers well-being as a possible focus for reorienting 21st century public policy, including its environmental dimension (WHO, 2013a).
Multilateral environmental agreements, such as those related to chemicals (UNEP, 2012b), are also of direct relevance to human health and well-being. The Rio+20 outcome document defines human health as 'a precondition for and an outcome and indicator of all three dimensions of sustainable development' (UN, 2012a).
|
Topic
|
Overarching strategies
|
Directives (examples)
|
|
Air
|
EU Thematic Strategy on air pollution
EU Clean Air Policy Package
|
Ambient Air Quality Directives
National Emission Ceilings Directive
|
|
Water
|
The Water Framework Directive
A Blueprint to Safeguard Europe's Water Resources
|
Drinking Water Directives
Urban Waste Water Treatment Directive
Bathing Water Directive
The Directive on Environmental Quality Standards
|
|
Noise
|
|
The Environmental Noise Directive
|
|
Chemicals
|
Registration, Evaluation, Authorisation and restriction of Chemicals regulation
Thematic Strategy on the sustainable use of pesticides
|
Directive establishing a framework for Community action to achieve the sustainable use of pesticides
Classification, Labelling and Packaging Regulation
Regulation concerning the making available on the market and use of biocidal products
Regulation concerning the placing of plant protection products on the market
|
|
Climate
|
EU Strategy on adaptation to climate change
Green Infrastructure — Enhancing Europe's Natural Capital
|
|
5.3 Environmental, demographic and lifestyle changes contribute to major health challenges
Various demographic and socio-economic trends, combined with persistent inequalities, affect the European population's vulnerability to multiple pressures, including those related to environment and climate.
EU citizens live longer than in many other parts of the world. Life expectancy at birth in the EU-28 exceeded 80 years in 2012, and is higher for women. The gap between the lowest life expectancy (68.4 years for men in Lithuania) and the highest (85.5 years for women in Spain) in the EU is considerable. The expected years lived without disability, as measured by healthy life years at birth, does not exceed 62 years in the EU-28 (EC, 2014f).
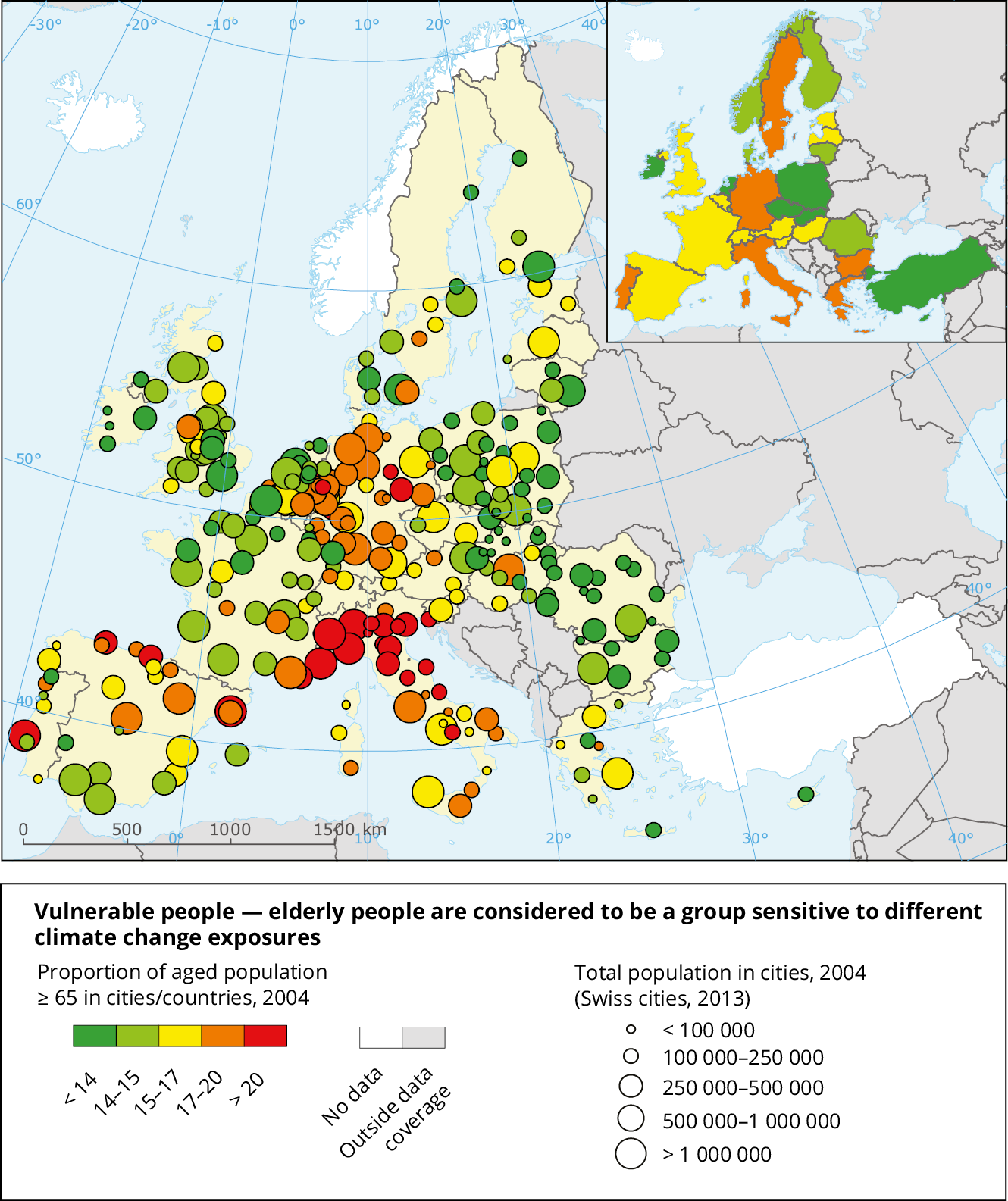
The share of the older population in the EU-27 has been increasing in recent years. The current proportion of people aged 65 years and over, already exceeds 17.5% and is projected to reach 29.5% by 2060 (Eurostat, 2008, 2010, 2011) (Map 5.1).
The leading causes of poor health in Europe are cardiovascular and respiratory diseases, cancer, diabetes, obesity, and mental disorders (IHME, 2013). Neuro-developmental disorders in children and reproductive problems are of growing concern, along with the emergence of communicable, vector-borne diseases, especially in the context of climate change and globalisation (ECDC, 2012c, 2013). The factors driving these growing public health issues are not sufficiently understood. Exposure to environmental factors certainly plays a role, but the complex causal pathways and interactions with demography or lifestyle factors are poorly understood. More knowledge is needed to effectively tackle these challenges (Balbus et al., 2013; Vineis et al., 2014; EEA/JRC, 2013).
The unequal distribution of environment-related costs and benefits across society is another important factor. Evidence is growing that environment-related inequalities and their potential impacts on health and well-being are strongly related to socio-economic factors, and to coping and adaptation capacities (Marmot et al., 2010; WHO, 2012; EEA/JRC, 2013). Furthermore, poor environmental conditions tend to be associated with social stressors (such as poverty, violence, etc.). However, little is known about the combined health effects of stress and pollution (Clougherty and Kubzansky, 2009; Clougherty et al., 2007).
Factors such as housing, food, mobility, and recreation affect both environmental pressures and human exposure to them. Lifestyles and consumption patterns, partly shaped by individual choices, play an important role here. In the long term, maintaining human health may increasingly depend on finding ways to meet societal needs at much lower environmental costs. Further efforts to improve the quality of the environment will therefore need to combine pollution abatement measures with incentives for resource-efficient production systems and sustainable consumption patterns.
5.4 Water availability has generally improved, but pollution and scarcity still cause health problems
The quantitative, ecological and chemical status of European waters can significantly affect human health and well-being (see also Section 3.5). These health effects can be felt directly, through lack of access to good quality drinking water, inadequate sanitation, exposure to contaminated bathing water, and consumption of contaminated freshwater and seafood. They can also be felt indirectly, when the ability of ecosystems to provide essential services for human well-being is undermined. The overall burden of water-borne diseases in Europe is probably underestimated (EFSA, 2013), and is likely to be affected by climate change (WHO, 2008; IPCC, 2014a).
Most Europeans receive treated drinking water from municipal supply systems, compliant with the quality standards set by the Drinking Water Directive (EU, 1998). Smaller water supplies, which serve some 22% of the EU population and have lower compliance with the quality standards (KWR, 2011), are more prone to contamination and to impacts of climate change. Special efforts are needed to improve the compliance of these smaller water supplies with Drinking Water Directive standards and to become resilient to climate change (EEA, 2011f; WHO, 2011c, 2010b).
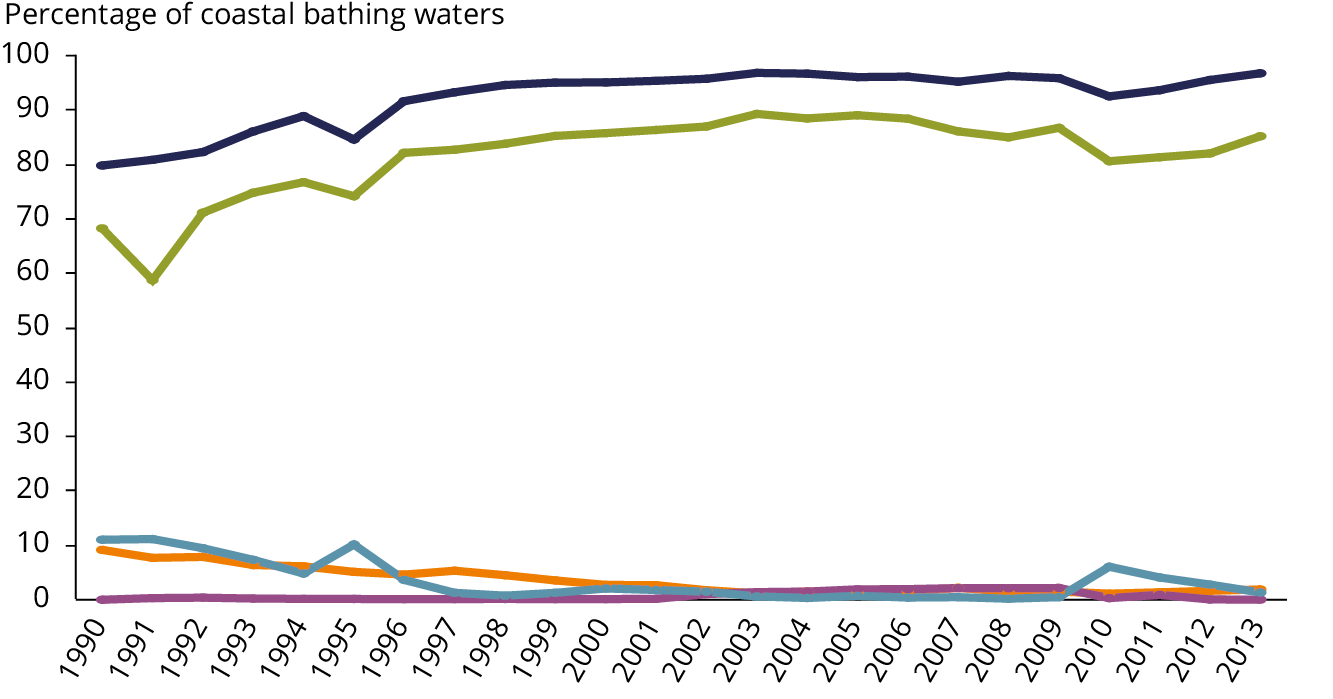
Progress in collecting and treating wastewater in Europe since the 1990s, under the Urban Waste Water Treatment Directive (EU, 1991), together with national legislation, has contributed to a sizeable improvement in bathing water quality, and reduced public health risks in parts of Europe (EEA, 2014g) (Figure 5.1).
Note: The figure shows the bathing water quality in European countries over time: 1990, 7 EU Member States; 1991 to 1994, 12 EU Member States; 1995–1996, 14 EU Member States; 1997 to 2003, 15 EU Member States; 2004, 21 EU Member States; 2005–2006, 25 EU Member States; 2007 to 2011, 27 EU Member States. Five Member States (Austria, the Czech Republic, Hungary, Luxembourg and Slovakia) have no coastal bathing waters. The quality classes under the New Bathing Water Directive (2006/7/EC) are jointed with compliance categories under the Bathing Water Directive (76/160/EEC).
Source: Indicator: Bathing water quality (CSI 022), EEA, 2014g.
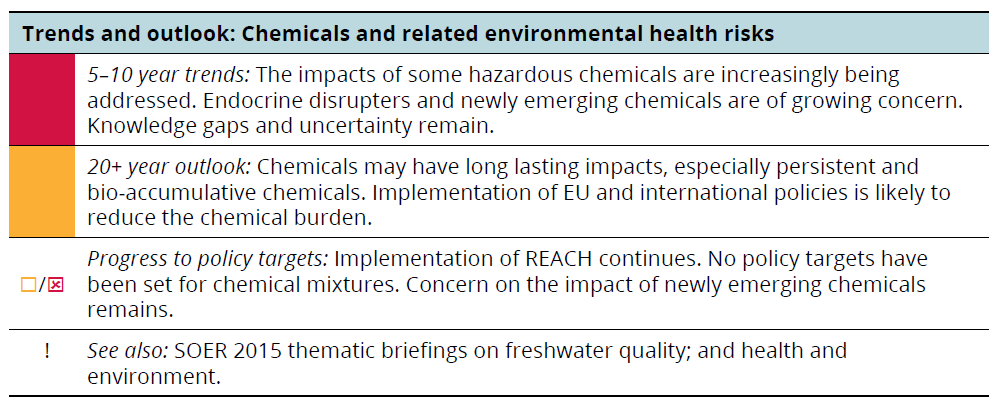
Despite considerable progress in reducing the discharge of pollutants into Europe's waters in recent decades, nutrients, pesticides, industrial chemicals, and household chemicals continue to affect the quality of surface, ground and marine waters. This threatens aquatic ecosystems and raises concern about potential human health impacts (EEA, 2011d; ETC/ICM, 2013) (see also Sections 3.5 and 3.6).
Chemicals from pharmaceuticals, personal care products, and other consumer products can have adverse effects on the environment and on human health. Endocrine disruption, which impacts the body's hormonal system, is of particular concern. Unfortunately, the environmental pathways and potential human health impacts of these chemicals are poorly understood, especially when people are exposed to mixtures of chemicals, or when exposure occurs in vulnerable population groups such as pregnant women, small children and people suffering from certain diseases (EEA, 2011d; Larsson et al., 2007; EEA, 2012f; EEA/JRC, 2013). Reducing chemical pollution at source has become an important resource efficiency measure, as advanced wastewater treatment and treatment of drinking water is energy and chemicals intensive.
Algal blooms and the associated proliferation of toxin-producing cyanobacteria are linked to nutrient enrichment of water bodies, especially during hot weather, with possible human health impacts (Jöhnk et al., 2008; Lucentini et al., 2009). Climate change can increase the frequency of harmful algal blooms and the growth of cyanobacteria, as well as the growth of other pathogenic microorganisms (Baker-Austin et al., 2012; IPCC, 2014a).
Meanwhile, water scarcity and drought are issues of increasing concern, with potentially severe consequences for agriculture, energy, tourism, and drinking water provision. Water shortages are projected to increase with climate change, particularly in the Mediterranean region (EEA, 2012h, 2012a). The resulting low flows can increase concentrations of biological and chemical contaminants (EEA, 2013c). Towns and cities can come to rely increasingly on groundwater to provide secure access to freshwater (EEA, 2012j). This raises sustainability concerns because groundwater resources often replenish slowly. Indirect climate change effects on water resources include impacts on animal health, food production, and ecosystem functioning (WHO, 2010b; IPCC, 2014a).
5.5 Ambient air quality has improved, but many citizens are still exposed to dangerous pollutants
Air pollution can damage human health through direct exposure via inhalation or indirectly through exposure to contaminants transported through the air, deposited on plants and the soil, and accumulated in the food chain. Air pollution continues to contribute to much of the burden of lung cancer, and respiratory and cardiovascular diseases in Europe (WHO, 2006, 2013b; IARC, 2012, 2013). The evidence is growing for other health effects, including reduced foetal growth and pre-term birth in children exposed prenatally, and impacts on health in adult life from perinatal exposure (WHO, 2013b; EEA/JRC, 2013).
The EU has introduced and implemented a range of legal instruments to improve air quality. Measures to combat pollution at source, and further implementation of the proposed Clean Air Package, in line with the latest knowledge, are expected to result in further improvement in air quality and in reduced health impacts by 2030 (EU, 2013).
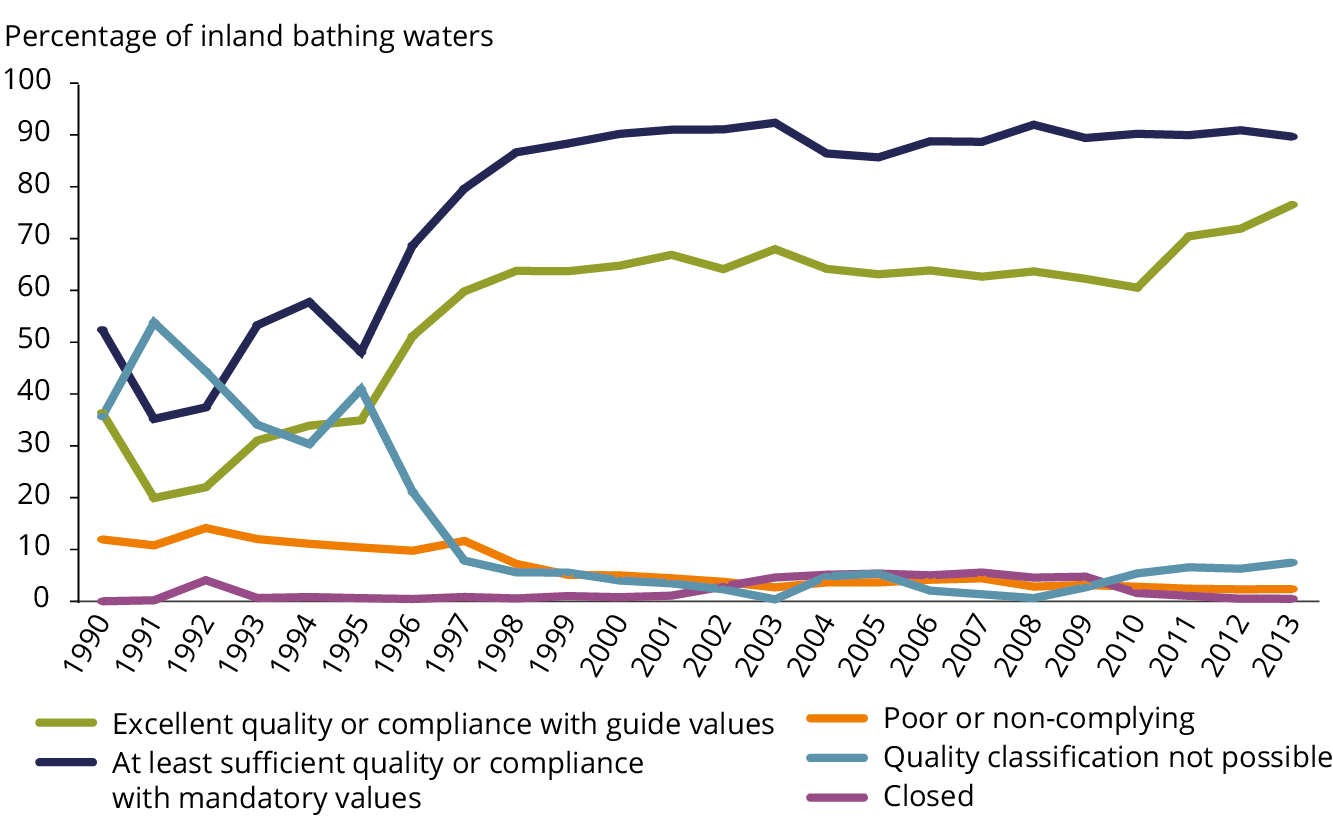
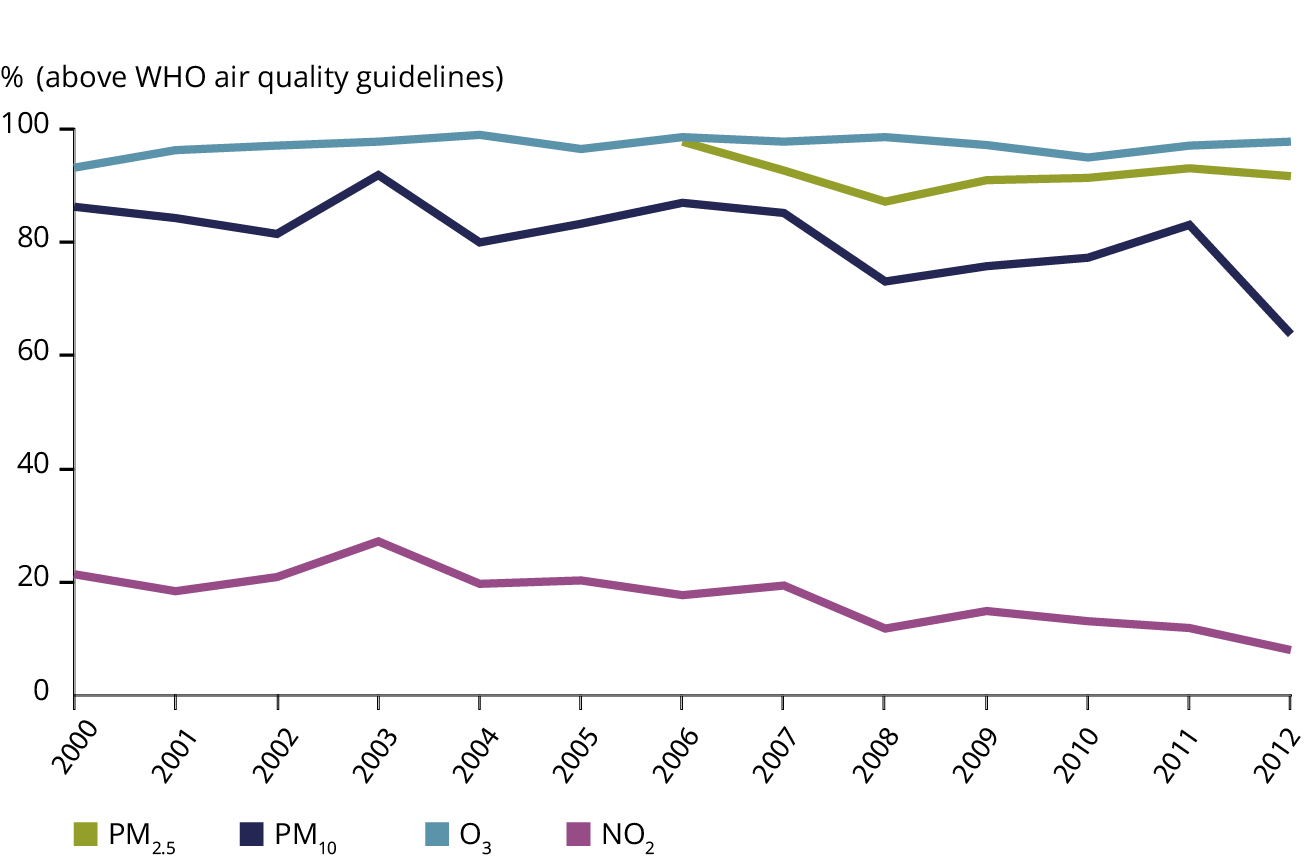
The situation regarding pollutants such as lead, sulphur dioxide and benzene has improved. Other pollutants remain of particular health concern. These include particulate matter (PM), for which no lower threshold for health effects has yet been established, ground-level ozone (O3), nitrogen dioxide (NO2), and carcinogenic polycyclic hydrocarbons, such as benzo(a)pyrene (BaP) (WHO, 2006). A significant proportion of Europe's urban population remains exposed to harmful levels of air pollution (Figure 5.2). The exposure of Europe's population becomes even more evident when using the exposure estimates based on World Health Organization air quality guidelines (WHO, 2006), which are more stringent than EU air quality standards for most regulated pollutants (EEA, 2014a).
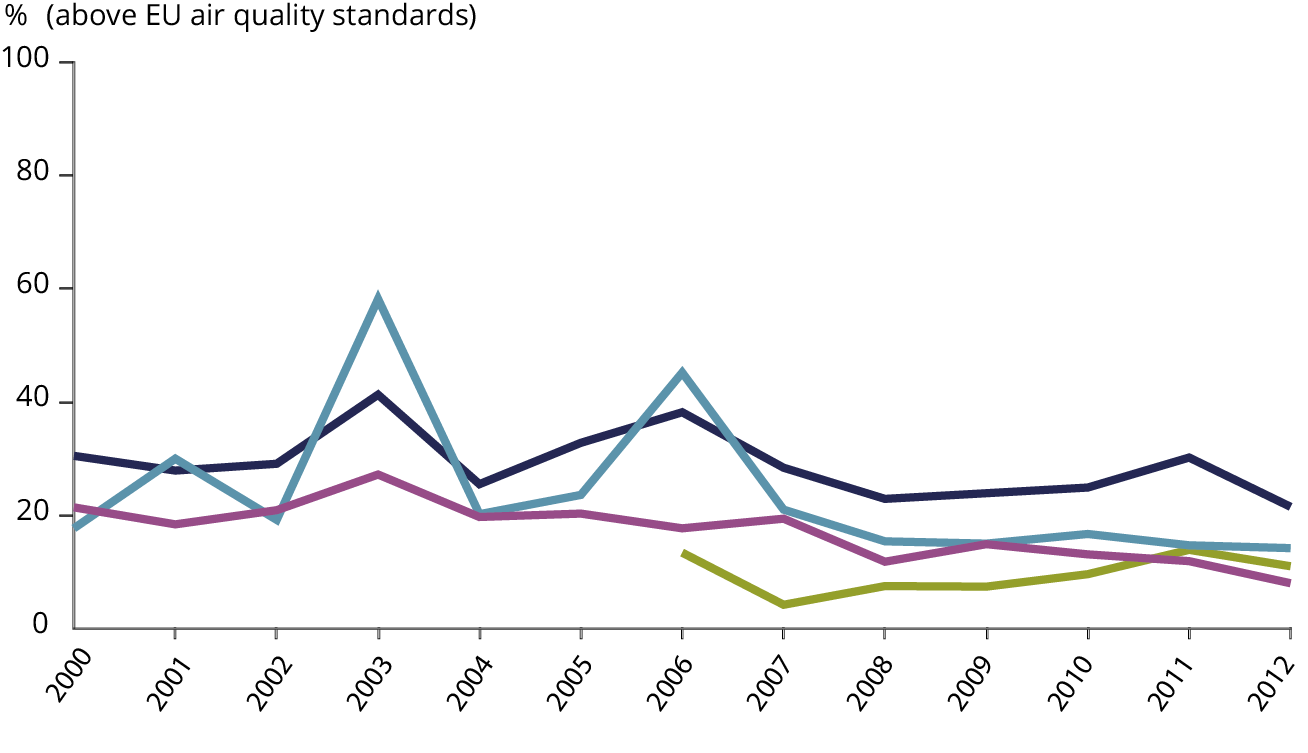
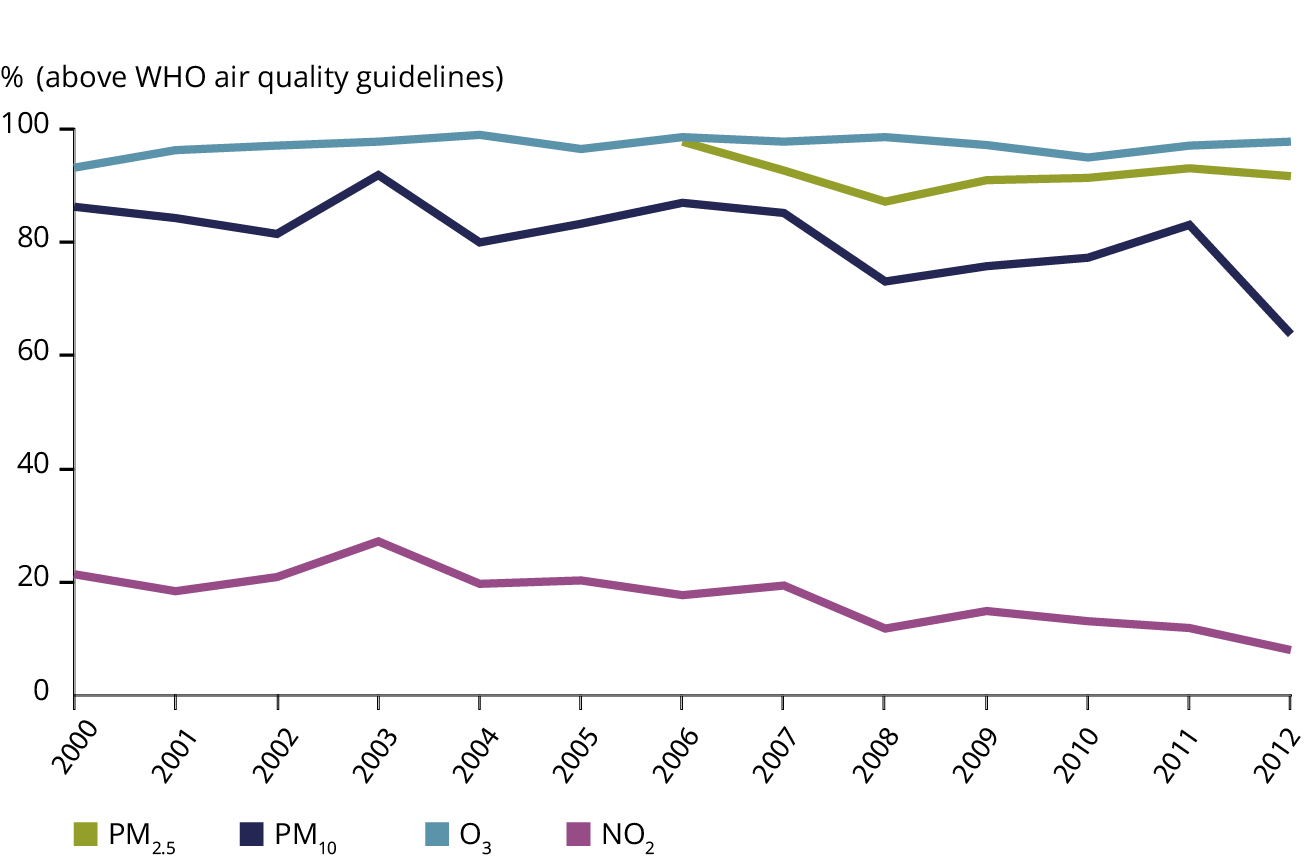
Note: For further details on the methodological approach, see CSI 004.
Source: CSI 004, EEA, 2014a.
Vehicles, industry, power plants, agriculture and households contribute to Europe's air pollution. Transport remains a main contributor to poor air quality levels in cities and related health impacts. Increasing traffic volumes, coupled with the promotion of diesel vehicles have played a role in this (EEA, 2013b; Global Road Safety Facility et al., 2014). Fundamental changes in the transport system, including technological solutions and behavioural change are needed to reduce its harmful impacts (see also Section 4.7).
The transboundary nature of particulate matter and ozone pollution requires national as well as international efforts to reduce emissions of precursor pollutants such as nitrogen oxides, ammonia and volatile organic compounds.
Another important source of particulate matter and polycyclic aromatic hydrocarbons is coal and wood burning for heating, in households as well as in commercial and institutional facilities. Low-level household emissions can significantly affect the concentrations close to the ground. Emissions of benzo(a)pyrene increased by 21% between 2003 and 2012, driven by the increase (24%) in emissions from domestic combustion in Europe. Exposure to benzo(a)pyrene is widespread, especially in central and eastern Europe. In 2012, some 25% of the EU urban population was exposed to benzo(a)pyrene concentrations above the EU target value. When estimated against the WHO air quality guidelines, as much as 88% of the EU urban population was exposed to benzo(a)pyrene concentrations above the reference level (EEA, 2014a).
Available estimates of health impacts of air pollution may vary due to different assumptions and some methodological issues(7). The European Commission estimated that health impacts of exposure to particulate matter could have declined by up to 20% between 2000 and 2010 (EU, 2013). Nevertheless, the toll of air pollution on health remains substantial. The EEA assessed that in 2011, about 430 000 premature deaths in the EU-28 were attributed to fine particulate matter (PM2.5), while the estimated impact of exposure to O3 concentrations exceeded 16 000 premature deaths per year(8) (EEA, 2014a).
Robust estimates are lacking for the less severe but more widespread impacts of air pollution, such as hospitalisations or use of medication. The existing assessments are based mainly on single-pollutant approaches, whereas air pollution actually comprises a complex mixture of chemical components that interact to produce impacts on human health (WHO, 2013b). Furthermore, concentrations of pollutants may vary due to meteorology, as dispersion and atmospheric conditions differ from year to year.
The quality of indoor air is also affected by ambient air quality, combustion processes, consumer products, energy efficiency improvements in buildings, and human behaviour. Exposure to indoor chemicals and biological agents has been linked to respiratory symptoms, allergies, asthma, and impacts on the immunological system (WHO, 2009a, 2010c, 2009c). Radon, a gas naturally present in the earth that leaks into buildings, is a well-established carcinogen. Exposure to this dangerous indoor air pollutant can occur underground or in poorly ventilated indoor environments. Although European citizens spend more than 85% of their time indoors, there is currently no dedicated policy framework that bridges safety, health, energy efficiency and sustainability (EEA/JRC, 2013).
5.6 Exposure to noise is a major health concern in urban areas
Noise pollution has long been recognised as a quality of life and well-being issue, but is increasingly being recognised as a public health issue. Road traffic is the greatest contributor to noise exposure in Europe. While its potential to contribute to harmful impacts is clear, tackling noise pollution is challenging, as it is a direct consequence of society's demand and need for mobility and productivity.
The Environmental Noise Directive (EU, 2002) requires EU Member States to undertake noise mapping (producing results in terms of common indicators) and to prepare action plans based on the noise maps. These action plans also aim to protect urban quiet areas against an increase in noise.
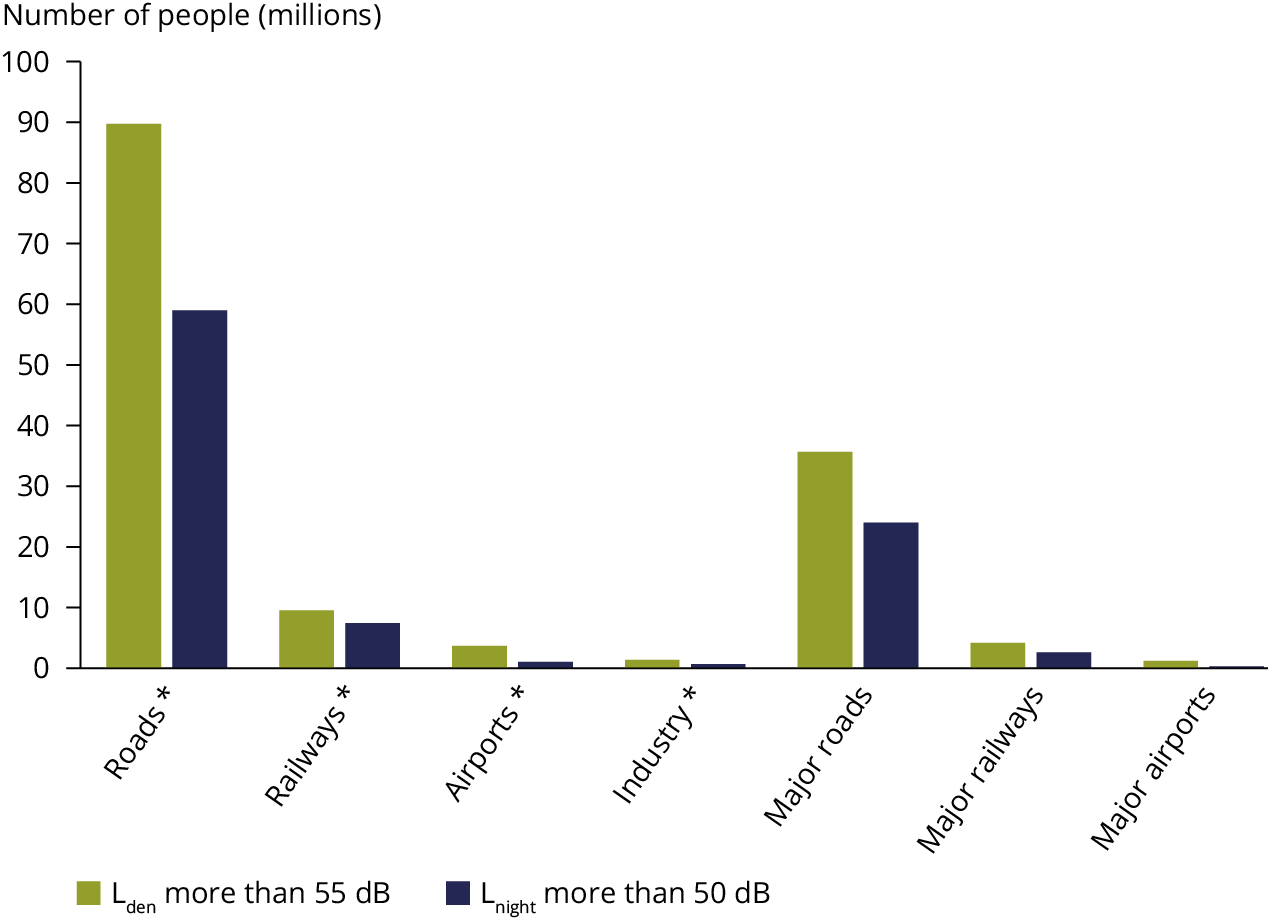
In 2011, at least 125 million people were estimated as being exposed to high levels of road traffic noise above the Lden(9) noise indicator of 55 dB (EEA, 2014p). In addition, many people were also exposed to rail, aircraft, and industrial noise, particularly in towns and cities (Figure 5.3). The average exposure to noise (i.e. Lden above 55 dB and Lnight above 50 dB) in selected urban agglomerations remained broadly constant between 2006 and 2011 according to comparable data reported by countries for these two years.
Note: Based on data reported by countries by 28 August 2013. Noise mapping and assessment methods may differ by country. Gaps in reported information have been filled with expert estimates where necessary.
Source: EEA, 2014p.
Environmental noise is not only a source of annoyance; it has been linked with increased risk of cardiovascular diseases, including heart attack and stroke (WHO, 2009b; JRC, 2013). The European Environmental Burden of Disease for noise is estimated as being at least 1 million life years lost per year, based upon earlier noise exposure data for 2006 and for road traffic alone (WHO/JRC, 2011). Most recently, exposure to environmental noise has been estimated to contribute around 10 000 cases of premature deaths due to coronary heart disease and stroke each year, with almost 90% of the noise-related health impacts being associated with road traffic noise (EEA, 2014p). However, these numbers are likely to be largely underestimated, as many countries do not report complete data sets, an issue that prevents robust trend and exposure analysis.
Reduction of exposure to noise is an important public health measure that must be addressed by both European and local measures. Examples of local measures include installation of road or rail noise barriers, where appropriate, or managing flight movements around airport locations. However, the most effective actions are those that reduce noise at source, for example by decreasing noise emissions of individual vehicles by introducing quieter tyres.
Green areas can also assist in reducing urban noise levels. There are opportunities to rethink urban design, architecture and transport in order to improve the management of urban noise. A recently issued guide on good practice in quiet areas (EEA, 2014j) is designed to support cities and countries in their efforts. Opportunities to improve public awareness and citizen engagement would also benefit from being further strengthened (e.g. EEA, 2011c, 2011e).
There is also emerging evidence that environmental noise may interact with air pollution, leading to greater impacts on human health (Selander et al., 2009; JRC, 2013). This illustrates the value of considering integrated mitigation approaches that address common sources of both air pollution and noise, such as road transport.
Further efforts to significantly decrease noise pollution in Europe by 2020 will require an updated noise policy aligned with the latest scientific knowledge, as well as improvements in city design and measures to reduce noise at source (EU, 2013).
5.7 Urban systems are relatively resource efficient, but also create multiple exposure patterns
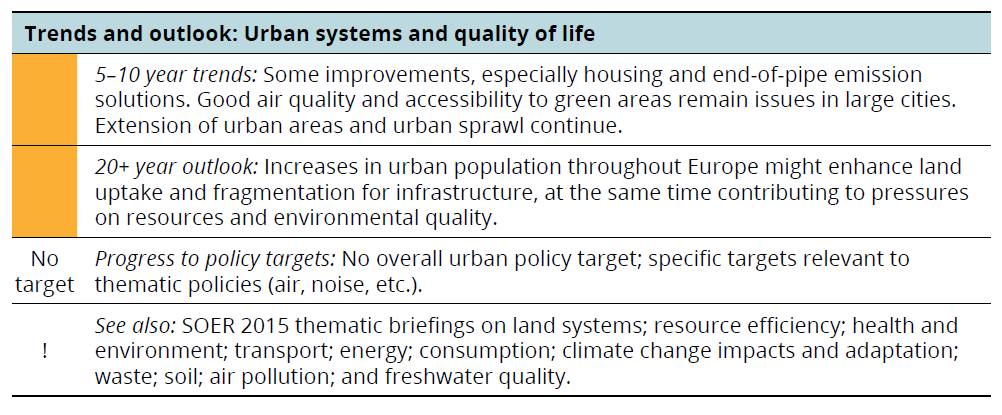
Nearly 73% of the European population lives in cities, and this is projected to reach 82% in 2050 (UN, 2011; 2012b). Urban development in Europe, particularly the increasing trend in peri-urbanisation, can increase pressures on the environment and human health, for example through landscape fragmentation and air emissions from transport (EEA, 2006; IPCC, 2014a) (see also Section 4.10).
Environmental impacts on human health and well-being are particularly pronounced in urban settings where multiple pressures coexist. This can affect large populations, including vulnerable groups, such as the very young and the elderly. Potential exacerbation of those impacts due to climate change points to a need for dedicated adaptation actions.
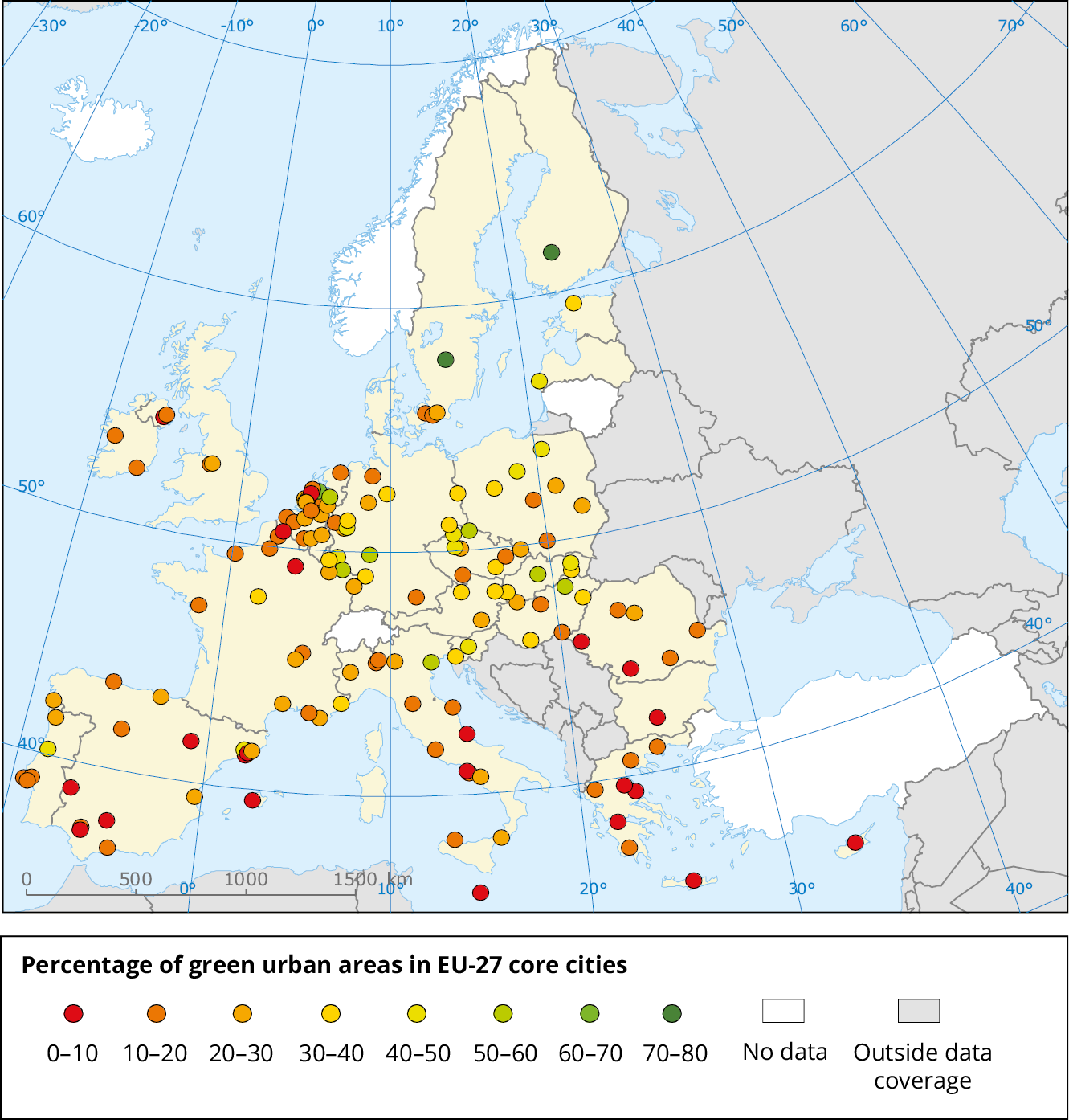
On the other hand, compact urban development and more resource-efficient approaches to the built environment provide opportunities to alleviate environmental pressures and enhance human well-being. In addition, well planned urban areas providing easy access to natural, green environments may deliver health and well-being benefits, including protection from the impacts of climate change (EEA, 2009a, 2012i; EEA/JRC, 2013).
The proportion of urban green space differs between European cities (Map 5.2). However, the actual use of green spaces depends critically on their accessibility, quality, safety, and size. There are also marked cultural and socio-demographic variations in the perception of green space and attitudes towards its use (EEA/JRC, 2013).
Note: Cities in their administrative borders (Eurostat, 2014i).
Source: EEA, 2010e.
The importance of urban green spaces for human health and well-being is increasingly recognised, partly due to better understanding of ecosystem services (Stone, 2009; Pretty et al., 2011). The benefits of high quality green environments to physical health, mental and social well-being, and improved quality of life can be substantial, although the nature of these interactions is not fully understood (EEA/JRC, 2013; Depledge and Bird, 2009; Greenspace Scotland, 2008; Paracchini et al., 2014). Fragmentary evidence indicates that access to green environments contributes to reducing (income-related) health inequalities (Mitchell and Popham, 2008; EEA/JRC, 2013).
The EU Green Infrastructure Strategy (EC, 2013b), and improved approaches to spatial analysis (EEA, 2014u), can contribute to assessing the trade-offs and co-benefits of urban development. Efforts to promote innovative urban policies for healthier, denser, greener and smarter cities are under way, for example by designating cities as European Green Capitals (EC, 2014g).
Multifunctional green infrastructure plays a role in urban adaptation to climate change, affecting temperature regulation, increased biodiversity, protection against noise, reduction of air pollution, prevention of soil erosion, and prevention of flooding (EC, 2013b; EEA, 2012i). The early integration of adaptation measures, including green infrastructure, into urban planning can offer long-term, cost-effective solutions. However, such measures are not yet widely implemented (EEA, 2012i; IPCC, 2014a) (see also Section 5.7).
Further implementation of policies for sustainable urban planning and design is crucial to enhance the sustainability of EU cities (EU, 2013). Smart planning and governance mechanisms can influence mobility patterns towards more sustainable forms of transport and reduced transport demand. They can also enhance the energy efficiency of buildings, reducing environmental pressures and improving well-being at the same time (EEA, 2013a, 2013f).
5.8 Health impacts of climate change require adaptation at different scales
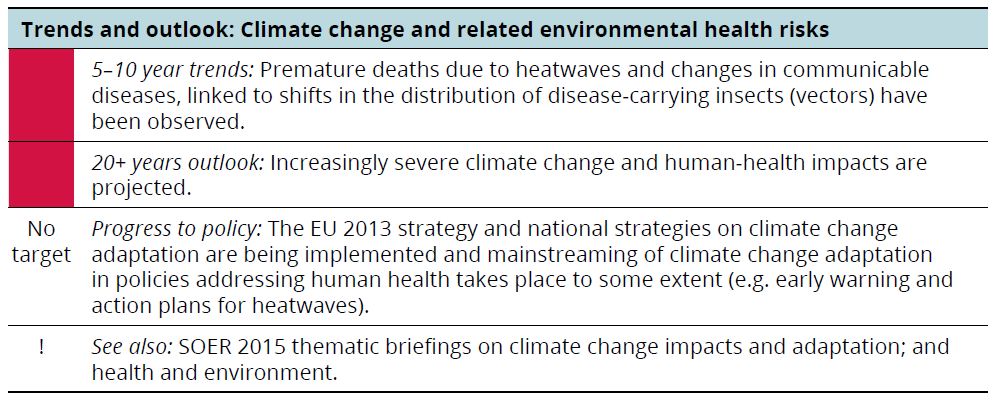
In Europe, the health and well-being impacts of climate change are related mainly to extreme weather events, changes in the distribution of climate-sensitive diseases, and changes in environmental and social conditions (EEA, 2012a; IPCC, 2014a; EEA, 2013e).
The impacts of both observed and projected climate change on human and natural systems in Europe are not distributed equally (EEA/JRC, 2013; EEA, 2013c) (see Section 3.9). To address these challenges, adaptation actions are needed, taking into account the contrasting vulnerabilities of different regions and societal groups (IPCC, 2014a). Vulnerable population groups include the elderly and children, people with chronic diseases, socially deprived groups and traditional societies. The Arctic, the Mediterranean basin, urban areas, mountain and coastal areas, and river flood-prone areas represent particularly vulnerable regions (EEA, 2012a, 2013c).
Climate-related extreme weather events, such as cold spells and heatwaves, exert health and social impacts in Europe (EEA, 2010a, 2012a). The likely increase in the frequency and intensity of heatwaves, particularly in southern Europe, is projected to increase heat-attributable deaths unless adaptation measures are undertaken (Baccini et al., 2011; WHO, 2011a; IPCC, 2014a). Without adaptation, between 60 000 and 165 000 additional heat-related deaths per year in the EU are projected by the 2080s, depending on the scenario (Ciscar et al., 2011).
The effects of heatwaves can be exacerbated in congested urban areas with high rates of soil sealing and heat-absorbing surfaces (EC, 2012a), insufficient nocturnal cooling, and poor air exchange (EEA, 2012i, 2012a). While most health impacts are likely to occur in urban areas, little is known on the possible effects of future changes in built infrastructure on the heat-related disease burden (IPCC, 2014a). Heatwave warning systems have been developed in many European countries (Lowe et al., 2011), but evidence of the effectiveness of such measures remains limited (WHO, 2011b; IPCC, 2014a).
Coherent approaches to urban adaptation combine so-called 'green', 'grey', and 'soft' measures (EEA, 2013c). Adaptation strategies for 'grey' infrastructure, such as buildings, transport, water utilities, or energy utilities need to ensure that this infrastructure continues to function in a more resource-efficient manner (IPCC, 2014a). Some adaptation actions can be governed at a city level, such as heatwave warning plans (an example of a 'soft' measure). Other actions may require multilevel governance mechanisms, involving regional, national or international levels, as in the case of flood protection (EEA, 2012i).
In the absence of adaptive measures, projected increases in coastal flood risk and river flood risk (linked to sea-level rise and increases in extreme precipitation) will substantially increase damages in terms of economic losses and people affected. Impacts on people's mental health, well-being, employment and mobility could be extensive and profound (WHO and PHE, 2013).
The anticipated impact of climate change on the distribution and seasonal pattern of some infectious diseases, including those transmitted by mosquitoes and ticks, suggests a need to improve response mechanisms (Semenza et al., 2011; Suk and Semenza, 2011; Lindgren et al., 2012; ECDC, 2012a). The ecological, social and economic factors need to be considered together with climate change, when planning adaptation and response measures.
The risks can be illustrated by the northward expansion of ticks and vector-borne diseases, or by the eastward and northward extension of the Asian tiger mosquito, which is a vector of several viruses currently present in southern Europe (ECDC, 2012b, 2012d, 2009; EEA/JRC, 2013). Climate change affects animal and plant diseases (IPCC, 2014a), and the likely knock-on impacts on biodiversity call for integrated, ecosystem-based response approaches (Araújo and Rahbek, 2006; EEA, 2012a). Air quality, distribution of allergenic pollen (such as ragweed), or other existing environmental quality problems can be exacerbated by climate change.
Unless adequately addressed, regional differences in health impacts and adaptation capacities can aggravate existing vulnerabilities and deepen socio-economic imbalances in Europe. For example, if climate change has more severe effects on the economies of southern Europe than in other regions, this might enhance the existing disparity between regions in Europe (EEA, 2012a, 2013c; IPCC, 2014a).
To address these challenges the EU has adopted a strategy on climate change adaptation that also includes actions related to human health. Several countries have developed national climate change adaptation strategies, including health strategies and action plans (Wolf et al., 2014). These include early warning systems for heatwaves and enhanced surveillance of infectious diseases.
5.9 Risk management needs to be adapted to emerging environment and health issues
Alongside persistent well known environmental health problems in Europe, new issues are emerging. These emerging health threats are typically linked with lifestyle changes, the rapid pace of global environmental change, and developments in knowledge and technology (see Chapter 2).
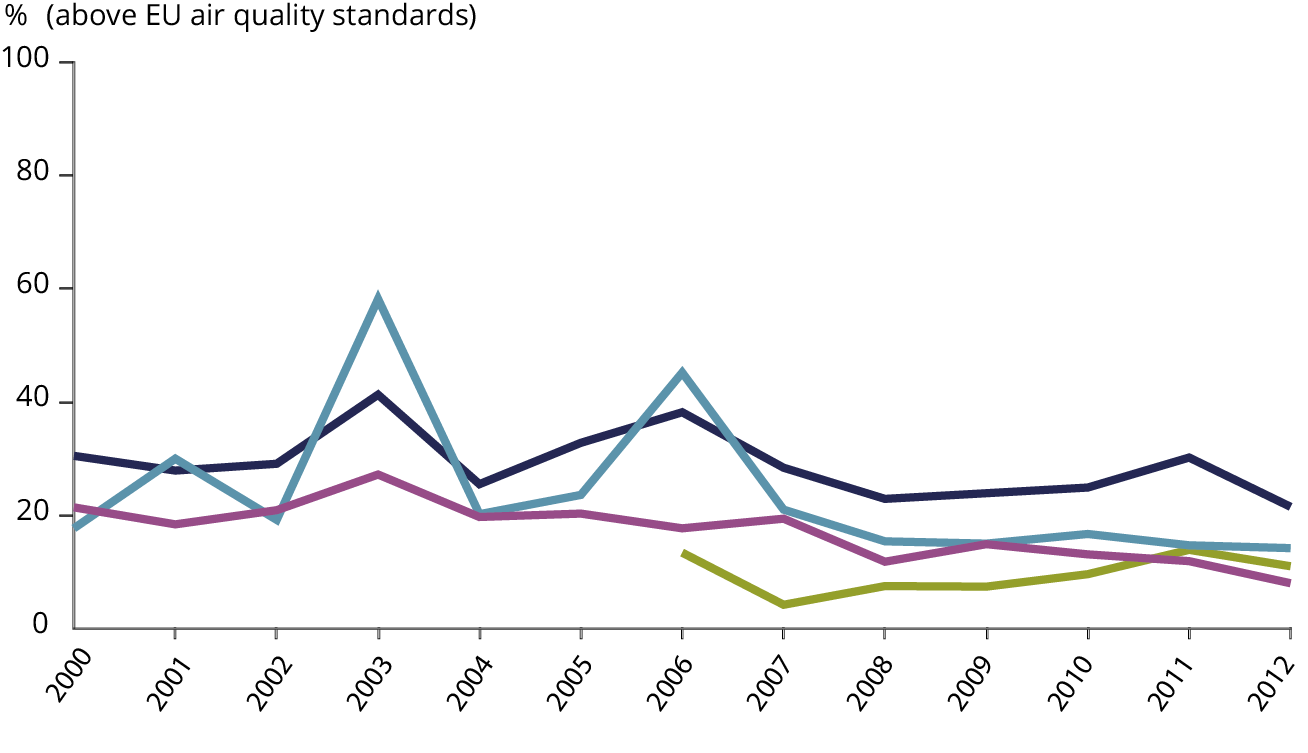
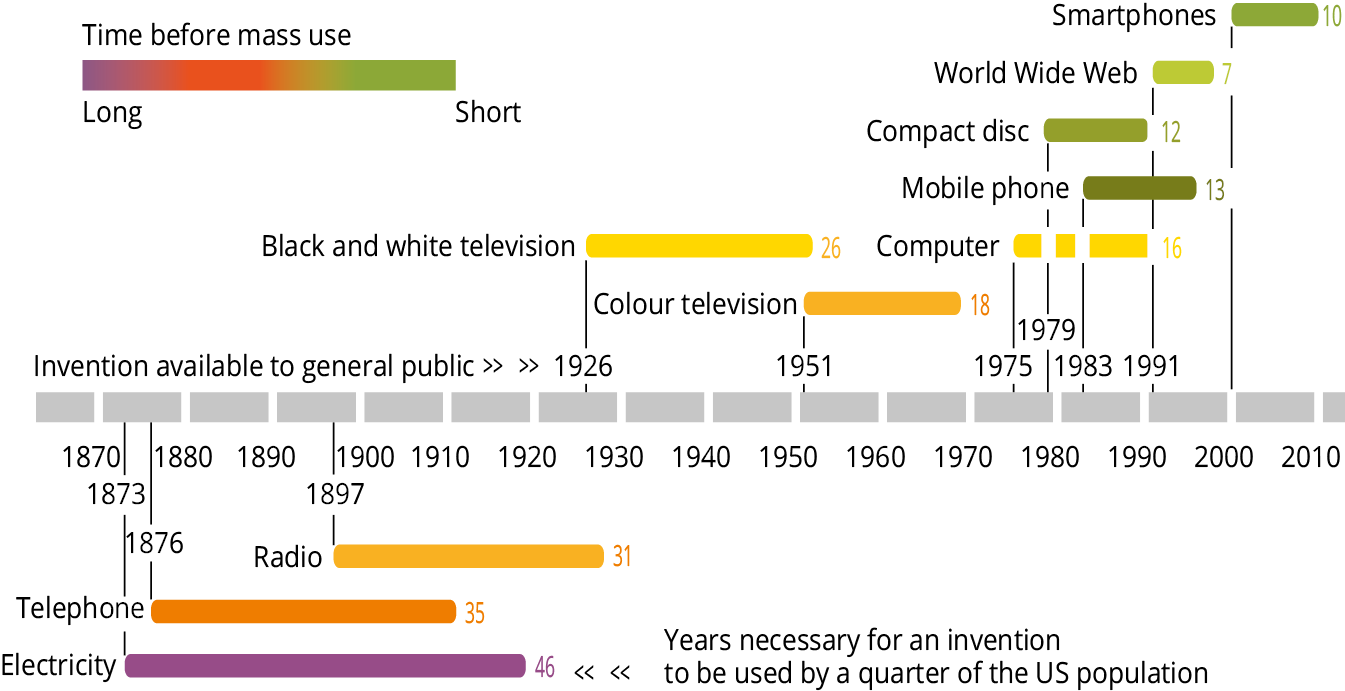
Technological developments have accelerated in recent years (Figure 5.4). Promising innovations, such as nanotechnology, synthetic biology and genetically modified organisms are being adopted by human society at an ever-increasing pace. As a result, people are exposed to a rapidly expanding array of substances and physical factors with largely unknown environmental and health effects. They include new chemicals and biological agents, light pollution and electromagnetic fields.
Source: Updated from EEA, 2010b, based on Kurzweil, 2005.
Chemicals in particular get growing attention in science and policy, due to their widespread occurrence and potential health impacts. According to the EU rapid alert system for non-food dangerous products (RAPEX), in 2013 chemical risks represented 20% of almost 2 400 notifications in different product categories, mainly in toys, textiles, clothing, and cosmetics (EC, 2014i).
One of the concerns is that low-level exposure of young children to certain mixtures of chemicals may affect health in adult life (Grandjean et al., 2008; Grandjean and Landrigan, 2014; Cohen Hubal et al., 2014). Particularly important in this regard are endocrine disrupting chemicals, which affect the body's hormonal system (WHO/UNEP, 2013). Several countries have already undertaken precautionary measures to reduce exposures to these chemicals, primarily in children and pregnant women (EEA/JRC, 2013), and endocrine disrupting chemicals are explicitly addressed in EU policy efforts towards creating a non-toxic environment (EU, 2013).
Exposure to mercury, a well-recognised toxic metal, also remains a public health concern in some parts of Europe, due to its effects on children's neurodevelopment (EEA/JRC, 2013). A new global convention on mercury (the Minamata convention) is expected to help gradually reduce that risk (UNEP, 2013). Consumption of contaminated seafood due to bio-accumulation of mercury and other persistent pollutants can pose health threats to vulnerable groups, such as pregnant women (EC, 2004b; EFSA, 2005; EEA/JRC, 2013).
A better understanding of complex exposure patterns, and how these patterns are linked to lifestyle and consumption behaviours is crucial to better tackle accumulative risks and prevent health impacts, especially in vulnerable population groups.
As for chemicals, there is increasing recognition that the current paradigm, which considers substances on a chemical by chemical basis under the assumption of linearity of exposure-response relationship, underestimates risks to human health and to the environment (Kortenkamp et al., 2012; EC, 2012c). Cumulative risk assessment is needed, taking account of vulnerable groups, multiple exposures, potential interactions between chemicals, and effects at low levels of exposure (Kortenkamp et al., 2012; Meek et al., 2011; OECD, 2002).
In general, exploring the implications of new technologies needs to take into account a wide range of social, ethical and environmental impacts, as well as the risks and benefits of taking different courses of action. Oversight mechanisms based on the precautionary principle can anticipate and manage problems and opportunities, responding quickly to changing knowledge and circumstances (EC, 2011d; Sutcliffe, 2011; EEA, 2013k). While there is still a great need for more knowledge (Box 5.2), in many cases there is justification for precautionary policy measures.
Major gaps exist in the scientific understanding of the impacts of chemicals on health, partly due to the scarcity of data. Human bio-monitoring (determining chemicals in blood, urine and other tissues) plays a crucial role in filling this data gap. It can provide an integrated measure of human exposure to chemicals from different sources and through the different environmental pathways that chemicals take.
National and Europe-wide efforts, such as the (COPHES/DEMOCOPHES, 2009) projects, generate high quality, comparable human bio-monitoring data. Such activities merit further support to enhance the information and knowledge base and to better plan preventive measures. Efforts are also under way towards improving the accessibility of existing information on chemicals in environmental media, food and feed, indoor air and consumer products.



Document Actions
Share with others