Introduction and main results
Negative
impacts of environmental stressors on health can range from mild psychological
effects (e.g. noise annoyance), to effects on morbidity such as asthma and increased
mortality. Properly targeted and followed-up environmental health policies,
such as the coal burning ban in Dublin (1990)
and the smoking ban in public places in Rome
(2005) have demonstrated significant and immediate population level reductions
in death and diseases. The highest environment related health benefits are
delivered by policies that target environmental stressors that greatly
contribute to the burden of disease (BoD). The environmental burden of disease
(EBD) can be expressed in Disability Adjusted Life Years (DALYs). DALYs
standardise health effects by expressing the number of affected people, the
duration and severity of the health effects in one number [1,2] (more information) (link to http://www.who.int/quantifying_ehimpacts/en/).
The
Multinational European EBoDE project (Environmental Burden of Disease in the
European region) has assessed the environmental burden of disease across six
countries: Belgium, Finland, France,
Germany, Italy and the Netherlands. The assessment implied
nine environmental stressors: benzene, dioxins (including furans and dioxin-like
PCBs), second-hand smoke, formaldehyde, lead, noise, ozone, particulate matter (PM)
and radon. This selection was based on the public health relevance, potential
for high individual risks, public concern and financial impacts of these
environmental stressors. The objectives of the project are to update previous EBD
assessments, to identify stressors relevant for the European region, to provide
harmonised EBD assessments for the participating countries, and to develop and
make available the methodology and databases for other countries.
Calculations
were based on the most recent scientific evidence concerning population
exposure and health effects, national exposure data, and WHO burden of disease
data and methods for estimating disease burden where available [3-5]. Even though the most recent scientific knowledge
and data were used, many uncertainties and controversies remain [6]. Results give only a crude ranking of
environmental health impacts and need to be interpreted with caution. The
preliminary results suggest that 3-7 % of the burden of disease in the
participating countries may be associated with the selected environmental
stressors (see Figure
1). Relatively, Finland
had the largest BoD and the smallest EBD, while for Italy this was vice versa. Particulate matter (PM) is estimated to be the leading
factor associated with 6 000 to 10 000 DALYs per million people,
followed by noise, radon and second-hand smoke (see Figure 2). Environmental health policies should focus
increasingly on these exposures.
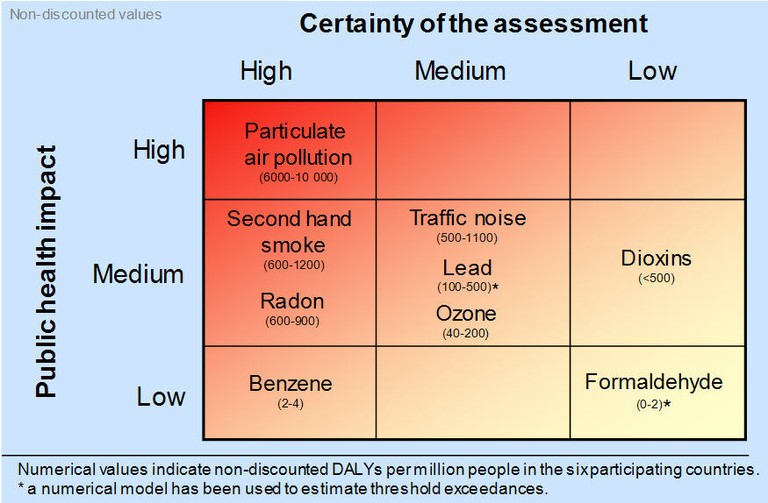
Figure 1: Relative
public health impact of the selected environmental stressors in the
participating countries. Numerical ranges reflect quantitative uncertainty in
the average estimate. Variability between countries is in many cases much
larger.
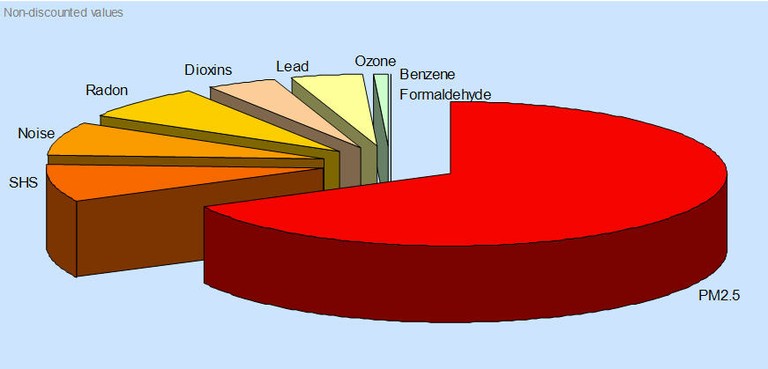
Figure 2: Relative
contribution of the nine selected environmental stressors to the total
environmental burden of disease attributable to these stressors (SHS = second-hand smoke).
Benzene
The use of benzene as an
additive in gasoline is now limited, but it is still used by industry in the
production of, for example, drugs and plastics. In addition, cigarette smoke
contains some benzene. Benzene is a known carcinogen for which no safe level of exposure can be recommended. The most significant adverse effects from prolonged
exposure to benzene are haematotoxicity, genotoxicity and carcinogenicity (IARC group 1 carcinogen) [7]. Increased mortality from leukaemia has been observed
in workers occupationally exposed. Based on the available information about leukaemia [8], the total impact of benzene on public health is
estimated to be low. Uncertainties relate mainly to the availability of exposure
data, exclusion of health effects other than leukaemia, and the potential
interaction of benzene with other components of tobacco smoke.
Dioxin
Dioxins
(including furans and dioxin-like PCBs) are a group of chemicals which are
considered to be highly toxic. They are by-products of various industrial
processes and combustion activities. Long-term exposure to dioxins has been
linked to effects on the immune system, the nervous system, the endocrine
system and reproductive functions [9]. In addition, chronic exposure may be related to
several types of cancer [10]. The relative burden of disease related to dioxins
is estimated to be medium, however, uncertainties are large. Effects of dioxins
cannot easily be distinguished from other occupational risk factors. Low-dose
effects are very difficult to assess, thresholds for effects are mostly unknown,
and exposure data are often only indirectly available. Our estimates only
include effects of dioxins on total cancer incidence. It is as yet unclear
whether our estimates over- or underestimate total health impacts.
Second-hand
smoke
Second-hand
smoke (SHS; also called environmental
tobacco smoke or passive smoking) is a known human carcinogen [11], causing lung cancer and a variety of other health
effects [12]. In our estimates, lower respiratory infections
and acute otitis media in young children, child asthma, adult asthma, lung
cancer and ischemic heart disease are included. Together, these health
endpoints are estimated to lead to 600–1200 DALYs per million people (medium
impact). Additional health effects supported by strong evidence, but for which
disease statistics were not available, or which would overlap with the assessed
outcomes, include sudden infant death syndrome, lower respiratory illness in
young children, low birth weight, reduced pulmonary function among children and
acute irritant symptoms and effects. In addition, uncertainties in our
estimates relate to, for example, indirect exposure measurements and relative
risks. Nonetheless, most evidence for SHS-related
impacts is fairly consistent, and the estimates of the burden of disease are
considered relatively stable.
Formaldehyde
Formaldehyde is
widely present, both indoors and outdoors, but it reaches high levels mostly
indoors. It is used in the production of several building materials and
household products, and it can be a by-product of combustion. Exposure to
formaldehyde may cause eye, nose, and throat irritation, may trigger asthma
attacks and may cause cancer [13]. The burden of disease related to formaldehyde, based
on asthma incidence in children below three years is estimated to be relatively
low. However, the consistency of the knowledge base is low, with uncertainties
related to the difficulty of establishing a threshold for effects, a lack of
epidemiological data and a large discrepancy in widely used models.
Lead
Exposure to
lead may cause, amongst other things, kidney damage, miscarriages, effects on the
nervous system, declined fertility, loss of IQ and behavioural disruptions [14,15]. Lead is present in the environment because of the
former use of lead in gasoline, leaded drinking water pipes, and the use of
lead in paints and other building materials. Exposure to lead has significantly
decreased for many countries in the last two decades. Indeed, lead has been the success story in environmental
policies, but the follow-up in exposure data in the general population is poor.
Also, current studies suggest that there is no ’safe‘ level of lead exposure. IARC rated lead and inorganic lead compounds as
probably carcinogenic to humans (Group 2A) in 2006 [16]. Lead has been estimated to contribute to 100–500
DALYs per million people (medium impact). These preliminary estimates are based
on a limited number of health endpoints, namely mild mental retardation
(children zero to four years) and hypertensive disease (adults). Other
uncertainties relate to the availability of dose-response functions over the
complete exposure spectrum, and the aggregation of effects.
Environmental noise
Exposure to
transport noise from road, rail, and air traffic affects a great number of
people, and may cause sleep disturbance as well as stress, leading e.g. to high
blood pressure and increased incidence of myocardial infarction [5,17-19]. Noise exposure has also been linked to effects on
cognition, but these are difficult to quantify and hence excluded from the
assessment. Our estimates include severe sleep disturbance and myocardial
infarction. Since so many people are exposed to noise, the total associated
disease burden, despite the relatively small disability weights, is
substantial. Important sources of uncertainties relate to incomplete exposure
data from environmental noise directive reporting, unavailable exposure-response-functions
for certain transport sources and health effects, and difficulty to establish thresholds for effects.
Ozone
Exposure to
ozone can lead to a variety of respiratory health effects, such as coughing,
throat irritation and reduced lung function. In addition, it can worsen
bronchitis, emphysema, and asthma [20]. The relative impact of ozone on public health is
medium, based on calculations which include total mortality, minor restricted
activity days, coughing in children and lower respiratory symptoms in children.
The selected morbidity health endpoints, which are based on the selection used
by the CAFE (Clean Air
For Europe) programme (link to: http://gains.iiasa.ac.at/index.php/policyapplications/cafe-clean-air-for-europe),
are estimated to account for 90 % of the total morbidity effects.
Uncertainties in the calculations relate, amongst other issues, to the
estimated number of years of life lost for mortality.
Particulate matter
Particulate
matter (PM) is identified in our analysis as the biggest contributor to the
total burden of disease. Exposure to PM has been associated with both
respiratory and cardiovascular effects. The body of evidence is fairly
consistent [5]. The health endpoints and dose-response models have
been selected based on the thorough review prepared for the CAFE programme (link to: http://gains.iiasa.ac.at/index.php/policyapplications/cafe-clean-air-for-europe).
Exposure data were derived using a combination of models and measurements. Remaining
uncertainties relate to the inclusion of PM from natural sources and sources
outside Europe (which are included in this
study), the exposure-response functions for e.g. chronic bronchitis, the
estimated number of years of life lost for mortality, and the potential of
double counting of morbidity effects by combining the restricted activity days
and lower respiratory symptom days.
Radon
Radon is a
short-lived radioactive gas that occurs naturally in soils and rocks because it
is generated by the radioactive decay of uranium. Indoor radon concentrations
differ based on the characteristics of the geological substrates beneath houses
and the use of different building materials. Exposure to radon has been
consistently linked to lung cancer [21]. For our estimates, the results of the recent
European EnVIE project (link to:
http://paginas.fe.up.pt/~envie/),
indoor air radon levels from the European Radon mapping project (link to: http://radonmapping.jrc.ec.europa.eu/)
and risk estimates from the Darby et al. 2005 meta-analysis [22] were used. Radon is estimated to contribute 600–900 DALYs per million
people in the participating countries.
Project websites:
http://www.euro.who.int/envhealth/data/20090108_1
http://en.opasnet.org/w/Ebode
References:
1. Murray CJ, Lopez AD. The Global Burden of Disease. Cambridge, MA: Harvard University
Press, 1996.
2. Prüss-Ustün, A and Corvalán, C. Preventing disease through healthy
environments. Towards an estimate of the environmental burden of disease.
2006. WHO.
3. Fewtrell, L., Kaufman, R, and Prüss-Ustün, A.
Lead: Assessing the environmental burden
of disease. Environmental burden of disease series No. 2. 2003. WHO.
4. Oberg, M, Jaakkola, M, Prüss-Ustün, A, and
Woodward, A. Second-hand smoke: Assessing
the burden of disease at national and local levels. 2010. Geneva, World
Health Organization.
5. WHO. Guidance
for health risk assessment of environmental noise. 2010. Bonn, World Health
Organization.
6. Knol AB, Petersen AC, van der Sluijs JP,
Lebret E. Dealing with uncertainties in
environmental burden of disease assessment. Environ Health 2009;8:21.
7. IARC. Monographs
on the Evaluation of Carcinogenic Risks to Humans: Some Industrial Chemicals
and Dyestuffs. 29. 1982. International Agency for Research on Cancer.
8. WHO. Air
quality guidelines for Europe; Second edition. 2000. Copenhagen, World
Health Organization, Regional Office for Europe. 91.
9. EPA (U.S.Environmental Protection Agency). Exposure and Human Health Reassessment of
2,3,7,8-Tetrachlorodibenzo-p-Dioxin
(TCDD) and Related Compounds Part II: Health Assessment for
2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) and Related Compounds. 200.
Environmental Protection Agency.
10. NAS. Dioxin
Reassessment. National Academy of Sciences (NAS) Review, draft. 2004.
National Academy of Sciences.
11. IARC. Monographs
on the Evaluation of Carcinogenic Risks to Humans: Tobacco Smoke and
Involuntary Smoking. 83. 2002. Lyon, International Agency for Research on
Cancer.
12. U.S.Department of Health and Human Services. The health consequences of involuntary
exposure to tobacco smoke. A report of the Surgeon General. 2006. Rockville (MD), USA, U. S. Department
of Health and Human Services.
13. IARC. Monographs
on the Evaluation of Carcinogenic Risks to Humans: Formaldehyde,
2-Butoxyethanol and 1-tert-Butoxypropan-2-ol. 88, 39-325. 2006. Lyon,
International Agency for Research on Cancer.
14. Khoury J YKBPBDCRDKBRGTRSNHSLWGGJRR. Low-level environmental lead exposure and
children's intellectual function: an international pooled analysis. . 2005
Jul;113(7):894-9. Environmental
Health Perspectives 2005;113:894-899.
15. WHO. Health
risks of heavy metals from long-range transboundary air pollution. 2007. Copenhagen, WHO Regional Office for
Europe.
16. IARC. Monographs
on the Evaluation of Carcinogenic Risks to Humans: Inorganic and organic lead
compounds. 87. 2006. Lyon, International Agency for Research on Cancer.
17. WHO. Transport-related
Health Effects with a Particular Focus on Children. Topic report: noise.
CONTRIBUTION TO THE UNECE - WHO TRANSPORT, HEALTH AND ENVIRONMENT PAN-EUROPEAN
PROGRAMME - THE PEP. Available at: http://www.euro.who.int/Document/trt/PEPNoise.pdf. 2000.
18. Babisch, W. Transportation Noise and Cardiovascular Risk: Review and Synthesis of
Epidemiological Studies, Dose-effect Curve and Risk Estimation. 2006.
Berlin, UBA.
19. Miedema H, Vos H. Associations between self-reported sleep disturbance and environmental
noise based on reanalyses of pooled data from 24 studies. Behavioural Sleep Medicine 2007;5:1-20.
20. WHO. Air
quality guidelines, Global update 2005.
2006. Copenhagen, WHO Regional Office for Europe.
21. WHO. WHO
handbook on indoor radon: A public health perspective. 2009. Geneva, World
Health Organization.
22. Darby S, Hill D, Auvinen A, Barros-Dios J,
Baysson H, Bochicchio F, Deo H, Falk R, Forastiere F, Hakama M, Heid I,
Kreienbrock L, Kreutzer M, Lagarde F, Mäkeläinen I, Muirhead C, Obereigner W,
Pershagen G, Ruano-Ravina A, Ruosteenoja E, Schaffrath-Rosario A, Tirmarche M,
Tomasek L, Whitley E, Wichmann HE, Doll R. Radon
in homes and lung cancer risk: collaborative analysis of individual data from
13 European case-control studies. British
Medical Journal 2005;330:223-226.
Participating institutes:
o
Flemish
Institute for Technological Research (VITO), Belgium
o
National
Institute for Health and Welfare (THL), Department of Environmental Health, Kuopio, Finland
o
French
Institute for Public Health Surveillance (InVS) , Paris, France
o
University
of Bielefeld, School
of Public Health, Department
‘Environment & Health’, Germany
o
NRW Institute of Health and Work, WHO Collaborating
Center for Regional Health Policy and Public Health, Bielefeld, Germany
o
Federal
Environment Agency (Umweltbundesamt), Berlin/Dessau-Roßlau, Germany
o
Department of
Occupational and Environmental Health, University
of Milan, Italy
o
Italian
National Health Institute, Rome,
Italy
o
National Institute of Public Health
and the Environment (RIVM), Bilthoven,
Netherlands
o
WHO, European
Centre for Environment and Health, Bonn,
Germany
o
WHO, Geneva, Switzerland
Document Actions
Share with others